Structural Disorders
Structural disorders, on the other hand, are those in which the bowel looks abnormal and doesn’t work properly. Symptoms can be similar to functional disorders, but may also include obstructed bowel movements, unexplained weight loss and fatigue, significant changes to bowel habits and unusual pain or even bleeding.
Sometimes, the structural abnormality needs to be removed surgically. Also, if not properly addressed, some structural disorders can even lead to more serious complications.
The most common structural disorders are those affecting the anus (e.g. haemorrhoids), as well as diverticular disease, colitis, and cancer to name a few.
1. Haemorrhoids
Haemorrhoids are swollen blood vessels that line the anal opening caused by chronic excess pressure from straining during a bowel movement, persistent diarrhoea, or pregnancy.
There are two types of haemorrhoids: internal and external.
Internal haemorrhoids
Internal haemorrhoids are normal structures cushioning the lower rectum and protecting it from damage by stool. When they fall down into the anus as a result of straining, they become irritated and start to bleed. Ultimately, internal haemorrhoids can fall down enough to prolapse (sink or protrude) out of the anus.
Treatment includes improving bowel habits (such as avoiding constipation, not straining during bowel movements, and moving your bowels when you have the urge), or if persistent, removing them surgically.
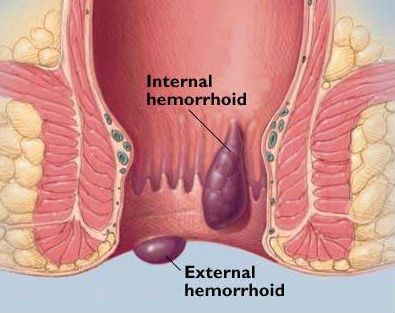
External haemorrhoids
External haemorrhoids are veins that lie just under the skin on the outside of the anus. Sometimes, after straining, the external haemorrhoidal veins burst and a blood clot forms under the skin. This very painful condition is called a pile.
Treatment includes removing the clot and vein under local anaesthesia in the doctor’s office.
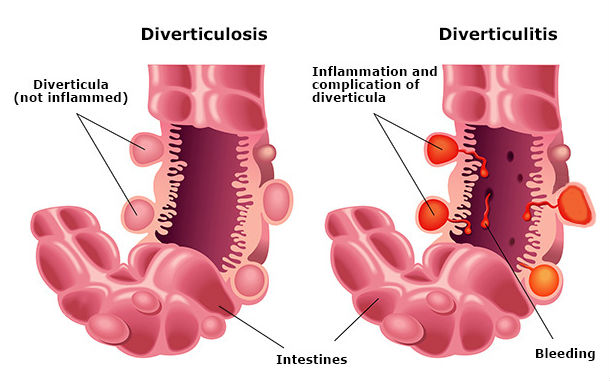
2. Diverticular disease
Diverticulosis is the presence of small outpouchings (diverticula) in the muscular wall of the large intestine that form in weakened areas of the bowel. They usually occur in the sigmoid colon, the high-pressure area of the lower large intestine.
Diverticular disease is very common and occurs in 10% of people over age 40 and in 50% of people over age 60 in Western cultures.
It is often caused by too little fibre in the diet.
Diverticulosis rarely causes symptoms. Complications of diverticular disease happen in about 10 percent of people with outpouchings.
They include infection or inflammation (diverticulitis), bleeding, and obstruction. Treatment of diverticulitis includes antibiotics, increased fluids, and a special diet. Surgery is needed in about half the patients who have complications to remove the involved segment of the colon.
3. Colitis
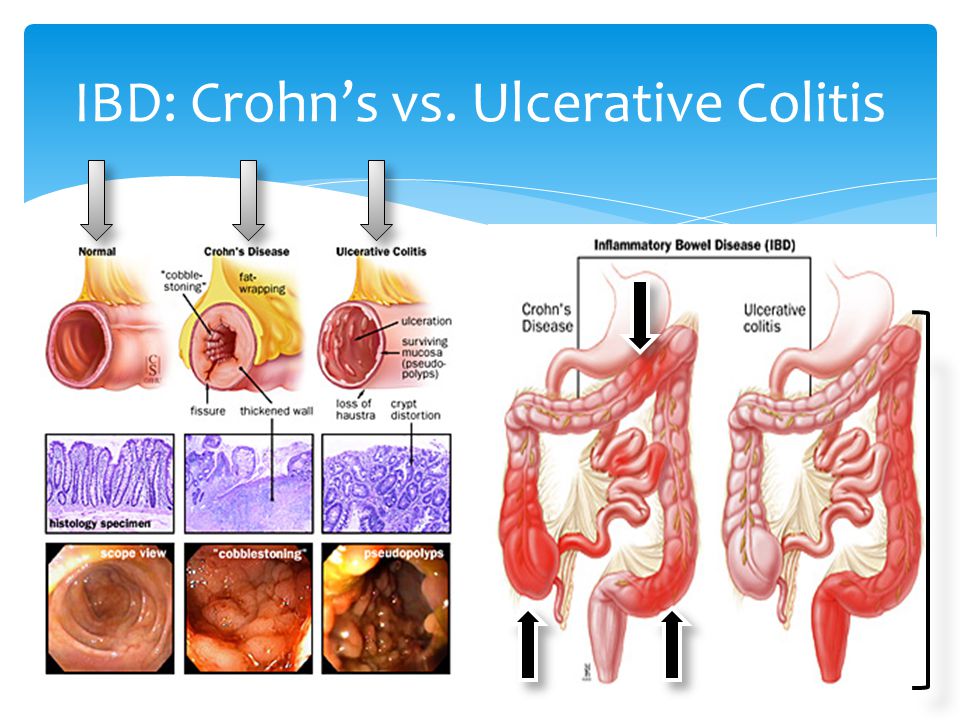
There are several types of colitis, conditions that cause inflammatory bowel disease (IBD), with the most common being ulcerative colitis and Crohn’s disease. The exact cause is still unknown, although diet and stress aggravate it.
Colitis causes diarrhoea, rectal bleeding, abdominal cramps, and urgency (frequent and immediate need to empty the bowels). Treatment depends on the diagnosis, which is made by colonoscopy and biopsy.
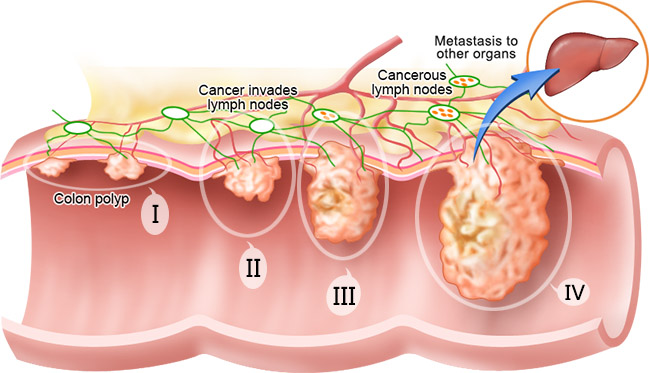
4. Colon cancer
Almost all colorectal cancers begin as polyps, benign (non-cancerous) growths in the tissues lining the colon and rectum. Cancer develops when these polyps grow and abnormal cells develop and start to invade surrounding tissue. Removal of polyps can prevent the development of colorectal cancer.
Most early forms of colorectal cancer do not cause symptoms, which makes screening especially important. When symptoms do occur, the cancer might already be quite advanced.
Symptoms include blood on or mixed in with the stool, a change in normal bowel habits, narrowing of the stool, abdominal pain, weight loss, or constant tiredness.
The good news is that the majority of gastrointestinal issues can be prevented, reduced or managed through healthy lifestyle and dietary choices, practicing good bowel habits, and receiving regular physical exams and cancer screenings.
Always remember that if you experience gastrointestinal issues that do not improve or worsen over time, see your health care provider to determine the cause of these issues and the best way to address them.