A Deeper Look Into Hashimoto’s Thyroiditis: The First Autoimmune Disease
Hashimoto’s thyroiditis was the first disease to be recognized as an autoimmune disease. It was first described by the Japanese specialist Hakaru Hashimoto in 1912.
So what exactly is happening in this thyroid disease?
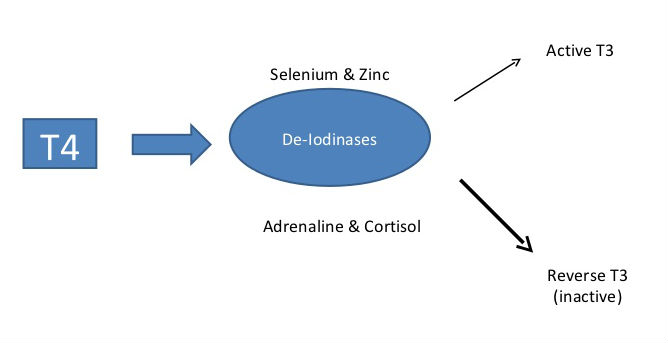
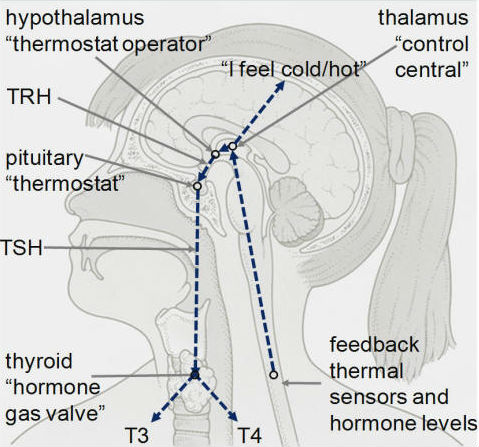
The pituitary gland produces a hormone called thyroid stimulating hormone (TSH), which prompts the thyroid to release thyroid hormones, mainly thyroxine (T4) and some triiodothyroxine (T3), into the bloodstream. T3 possesses about four times the hormone “strength” as T4.
T4 converts into the more active T3 in multiple tissues and organs, but especially in the liver, gut, skeletal muscle, brain and the thyroid gland itself. This conversion requires sufficient selenium and zinc levels. However, if elevated adrenaline and cortisol levels are present (from stress), reverse T3 is produced which is inactive.
Every cell in the body depends upon thyroid hormones for regulation of their metabolism. Thyroid hormones are responsible for the very important role of stimulating the metabolism of the foods we eat, and extracting vitamins and producing energy from food. They are also vital to the production of other hormones, as well as the growth and development of our nervous system.
A disturbance in thyroid function can therefore cause widespread, noticeable health problems.
MAJOR EFFECTS OF THYROID HORMONES IN THE BODY
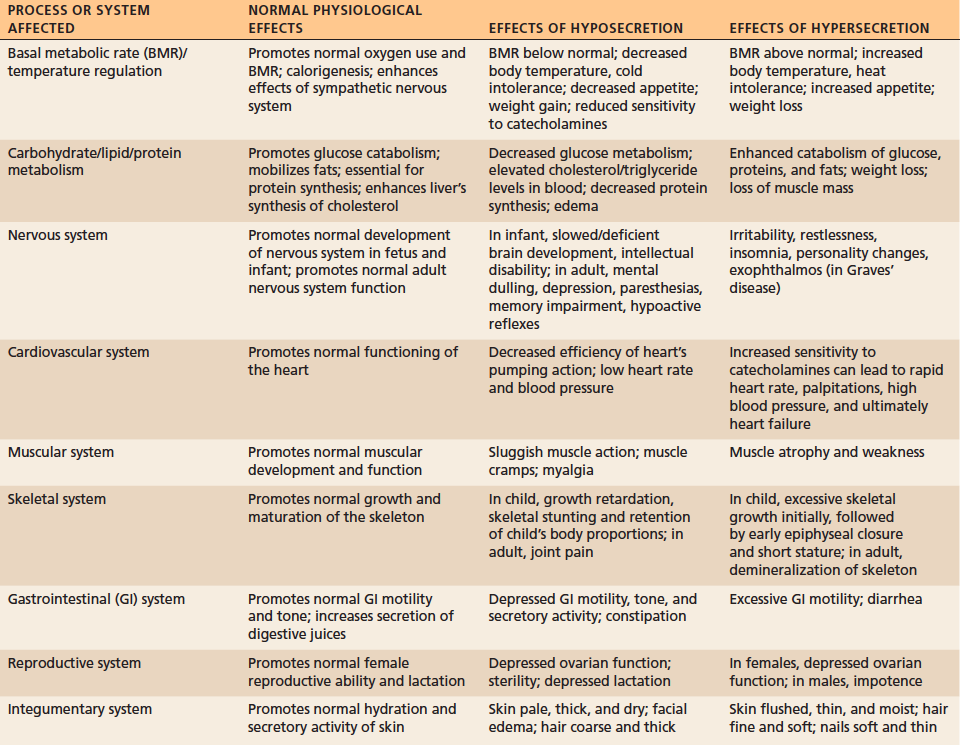
The thyroid has been called the “thermostat” of our body, as it maintains our temperature. The hypothalamus and pituitary gland communicate to the thyroid via feedback from thermal sensors and hormone levels. Indirectly, thyroid function affects every reaction in the human body, as the temperature has to be just right for these reactions to take place properly.
TEMPERATURE CONTROL IN THE BODY
Hypothyroidism is characterized as having an under-active thyroid gland that doesn’t properly make or release enough thyroid hormones. Hypothyroidism can be due to an iodine deficiency, thyroidectomy, a traumatic event, and even an immune attack.
Symptoms of hypothyroidism are vast and complex. These include:
- fatigue & exhaustion
- feeling run down & sluggish
- mood swings, depression & anxiety
- brain fog, poor concentration & forgetfulness
- lack of motivation & socially distant
- weight gain (especially belly fat) or inability to lose weight
- skin issues (dry, coarse, itchy), acne & eczema
- dry, coarse and/or thinning hair, eyebrow loss & brittle nails
- water retention & puffy eyes
- feeling cold (especially hands & feet)
- digestive discomfort, constipation/diarrhoea, acid reflux, gas & bloating
- candida overgrowth
- muscle aches, muscle cramps & muscle loss
- frequent colds
- throat discomfort and/or tightness
- hormone imbalance – low sex drive, PMS, irregular periods & infertility and/or miscarriages
- hypoglycaemia
- low levels of vitamin D, B12 and/or ferritin (anaemia)
- osteopenia or osteoporosis
- high cholesterol levels
- sleep disturbances
Hashimoto’s thyroiditis is an autoimmune condition in which the body’s own immune system attacks the thyroid, and it often results in hypothyroidism, but can bounce a patient back and forth between hypo- and hyperthyroidism symptoms.
It’s worth repeating this point just mentioned. Hashimoto’s is an autoimmune condition. If you have it, the problem is with your immune system, NOT your thyroid. The thyroid just happens to suffer from the autoimmune attack. In the case of Hashimoto’s (like all autoimmune diseases), it is the digestive tract that needs help and not the thyroid alone.
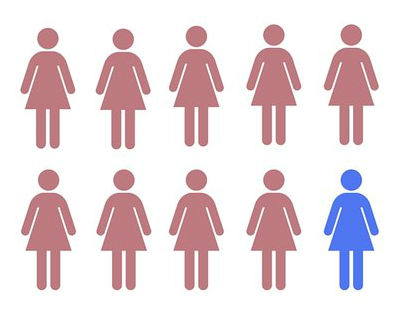
Interestingly, 90% of people with hypothyroidism have it due to Hashimoto’s disease. So when a patient is diagnosed with hypothyroidism, chances are it may in fact be an autoimmune disease.
More Than 9 Out Of 10
diagnosed with hypothyroidism have Hashimoto’s
Sadly, most of these patients go undiagnosed, because most doctors do not run the correct blood work (i.e. screening for Thyroid Peroxidase (TPO) and Thyroglobulin (TGB) antibodies) to check for autoimmune hypothyroidism. Also, treatment for hypothyroid or autoimmune hypothyroid is the same. Doctors give a standard T4 “replacement hormone”, which does very little if anything for the autoimmune type of hypothyroid.

TSH (Thyroid Stimulating Hormone) levels are considered the “gold standard” for thyroid testing and have been used as the gauge by doctors for telling patients that they should be feeling better. Many patients treated with thyroid replacement hormones achieve “normal” TSH levels and so the medications seem to be a “success”. Ironically, many of these patients still continue to suffer with a multitude of unexplainable symptoms.
A traditional “normal” TSH level is between 0.5-5.0 mIU/L, with anything above 5.0 mIU/L suggesting hypothyroidism. However, functional medicine practitioners suggest a lower TSH level between 0.5-2.0 mIU/L as the therapeutic target for optimal thyroid health and symptom relief. A TSH level above 2.0 mIU/L would be considered hypothyroid.
As a result of screening discrepancies, thyroid conditions remain the number one under-diagnosed and mistreated conditions in the world.
In addition, many patients are often suffering from adrenal fatigue AND hypothyroidism simultaneously, since the two organs are intimately connected, along with the gut. Adrenal fatigue leads to depleted levels of cortisol, our body’s natural anti-inflammatory agent. This causes an increased production of pro-inflammatory cytokines, resulting in immune system over-activation and inflammation. This inflammatory gut response leads to autoimmunity, via leaky gut.
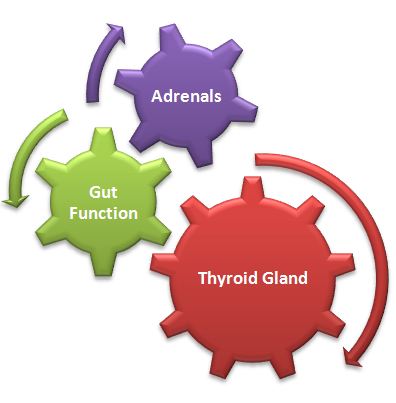
However, the patient is only treated for hypothyroidism alone. Over time this approach backfires and causes the adrenal fatigue condition to worsen.
It is important to understand that thyroid replacement medications increase the overall basal metabolic rate. The entire body is put into a state of over-drive. Pushing the adrenals in particular to work harder when they are already fatigued can unmask adrenal exhaustion or even trigger an adrenal crisis.
“With a broken engine (adrenals), you can press the accelerator pedal (thyroid) all you want, but you aren’t going anywhere!”
Weak adrenals are often associated with reduced availability of free thyroid hormone to the cells as well. As a result, symptoms of hypothyroidism often fail to improve over time and may in fact get worse with this single organ approach to healing, despite being placed on thyroid replacement therapy.
Doctors focusing on the thyroid alone without considering the adrenals frequently find themselves administering ever higher doses of thyroid replacement medication or switching from one medication to another without success. Doctors also find themselves treating stubborn symptoms, for conditions they believe are unrelated. However, the symptoms of adrenal fatigue and hypothyroidism are very similar.

When doctors are at a loss of what to do, they then prescribe anti-depressants, anti-anxiety agents, sleeping pills, blood pressure medication, antibiotics, steroids, and hormone replacement therapy.
Focusing on the thyroid without concurrent attention to the adrenals is a failed recovery strategy if adrenal fatigue is in fact the problem.
Fortunately, proper patient education, questioning and testing can accurately address a thyroid condition and any other underlying conditions. It is vital therefore to treat the whole patient and not treat the lab results instead.