You may have heard many times that “all disease begins in the gut”.
But what if I told you that … all disease actually begins in the MOUTH!
Let me explain further.
The human body has microbial colonies in many areas other than the intestinal system, and the ecology of these various microbial “communities” has a significant impact on many areas of health and disease.
One of the areas of the body inhabited by significant numbers of microbes that have recently been identified as having significant importance with regards to human health is the oral microbiome.
The Oral Microbiome
The oral microbiome is the complex and individualized bacteria colonies of our teeth, gums, tongue, cheeks, lips, and palates. The oral microbiome helps to maintain oral and systemic homeostasis and with over 700 species it is the largest microbiome after the large intestine. Oral microbiome dysbiosis is linked to dental caries and periodontitis, but research is now also emerging of the oral microbiome’s link to systemic health.

Determining If You Have An Unhealthy Oral Microbiome
An unhealthy oral microbiome can manifest as dental caries, gingivitis, periodontal disease, oral thrush, and halitosis. A trip to the dentist may be necessary to examine for caries and periodontal disease, however, signs that can easily be detected in a clinical setting include:
• Bleeding or inflamed gums
• Bad breath (halitosis)
• Loose or lost teeth
• Discoloration and plaque build-up on teeth
• White coating on the tongue or buccal surfaces

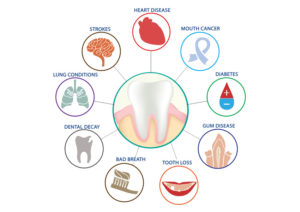
Oral Microbiome And Disease
Just like the microbiome of the gut, the oral microbiome thrives in an environment of diversity and beneficial bacteria for good dental health. The oral microbiome contains bacteria, but also archaea, protozoa, fungi, and beneficial viruses. The microbiome produces biofilm, a cover or shield which protects the colon. Dysbiosis of the oral microbiome due to a lack of diversity or presence of harmful bacteria can cause dental issues but is also implicated in physiological effects beyond the mouth.
Oral microbiome dysbiosis is linked to:
- Heart disease
- Stroke
- Lung conditions
- Preterm birth
- Increased risk of pregnancy gingivitis
- Gum disease
- Dental decay
- Root canals (such ‘dead teeth’ can cause infections in gums, jawline, and systemically)
- Gut, immune, endocrine, and nervous system (via the gut-brain axis)
- Mental & cognitive health (psychiatric disorders, anxiety, depression, Alzheimer’s disease)
- Infections (pneumonia & respiratory infections)
- Autoimmune disorders (Sjogren’s syndrome, systemic lupus erythematosus, Chrohn’s disease, and rheumatoid arthritis)
- Metabolic health (type 2 diabetes, obesity)
- Cancer
Mechanisms Leading To Disease
Oral microbial dysbiosis can affect health through the following actions:
- Activation of systemic inflammatory pathways
- Suppression of host immune responses
- Molecular mimicry
- Translocation of bacteria from the mouth into the systemic circulation
- Inflammation, pathogenic biofilm formation, and periodontal bone loss
- Increased systemic inflammation, immune activation, and infection of the cardiovascular system
- Inhaled oral bacteria into the respiratory system
- Loss of immune tolerance, activation of highly inflammatory cells, and increased systemic inflammation which is implicated in autoimmune disease
- Increased risk of developing type 2 diabetes mellitus, and in patients with diabetes, inflammation and hyperglycaemia predisposes and accelerates periodontal disease

Treatments For The Above
Patients with dental issues, oral inflammation, and connected diseases can be treated, in conjunction with their dentist, with a combination of lifestyle and dietary changes and the use of specific probiotics effective in improving oral health.
LIFESTYLE RECOMMENDATIONS:
- Tooth brushing and flossing twice a day
- Regular descaling at the dentist
- Quit smoking – the most impact in periodontal disease

DIETARY RECOMMENDATIONS:
Diet plays an important role in oral health with carbohydrate-rich foods having the most impact on oral pH. Consumption of sugars and starch can lead to bacterial fermentation in the mouth, which is highly acidic. Some suggestions include:
- Reduce processed carbohydrates
- Reduce sucrose and sugary drinks
- Reduce highly acidic foods – soft drinks, some fruit juices, vinegar, and dry wine
- Consume a whole foods diet – rich in fruits, vegetables, fibre, phytonutrients, minerals, and vitamins
- Reduce saturated fat (associated with periodontal disease) and increase omega-3 fats instead (reduces inflammation)
- Include prebiotics – an improved microbiome profile with the consumption of prebiotics

Probiotics
Specific probiotic strains can be used that beneficially impact the oral microbiome and oral health. In particular, two Lactobacillus reuteri strains (DSM 17938 and ATCC PTA 5289) are well-researched probiotic strains that have been shown to have many positive effects on oral health and the oral microbiome which includes:
- Prevention and treatment of dental caries
- Reduction in dental plaque build-up
- Prevention and treatment of gingivitis and periodontal disease
- Prevention and treatment of bad breath
- Reduction of oral candidiasis
- Reduce oral inflammation
- L. reuteri DSM 17938 produces reuterin, an antimicrobial metabolite that has antimicrobial, antiviral, and antifungal properties

L.reuteri DSM 17938 Benefits The Following Key Areas
1. Constipation
2. Functional abdominal pain
3. Gastroenteritis
4. GI pathogen overgrowth
5. SIBO
6. Antibiotic-associated side effects
7. Lactose intolerance
8. Reflux and regurgitation
9. Colic prevention and treatment
10. Infection protection
11. Reduces need for antibiotics
12. Allergy prevention and treatment
13. Infant immune support (particularly for infants born via C-section)
14. Immune modulation
15. Oral health management
In Summary
Rebalancing the oral microbiome is a key therapeutic target for anyone with dental caries and periodontitis. Addressing oral microbiome health is also an effective way to reduce risk factors for some chronic diseases. Lifestyle and dietary options along with regular dentist visits are vital to minimize any consequences of oral disease. Taking a probiotic such as Lactobacillus reuteri is a natural and effective option for addressing oral microbiome dysbiosis and restoring dysfunction.
For more information about improving your oral health, reach out to your holistic dentist or simply chat with me.
*If you’ve got this far – thank you for reading and I look forward to bringing you more information in the future.
Now, enjoy some basic information about good oral health…