I graduated as a pharmacist almost 30 years ago. I have seen a lot of changes in the pharmacy industry in that time. Indeed many have been exciting. There have been many advances with a multitude of new pharmaceuticals coming to market, helping to restore health to those in need.
I have also seen a great number of drugs withdrawn from the market due to their horrible side effects. Drugs that were prescribed by doctors who trusted the drug companies that convinced them of their safety.
Doctors are busy. They lack the time to look deeper into chronic disease states. Now, more than ever, doctors are having to treat complex symptoms in an average consult time of less than 10 minutes.
Patients want healing and relief of their complaints. They often put a lot of reasonability for their health onto their doctor, which is unreasonable at times. Consequently, doctors know only one thing to achieve that difficult goal …. ‘a pill for every ill’.
Many drugs are over-prescribed as a result of trying to meet this often unrealistic expectation of patients.
Perhaps one of the most commonly prescribed type of drugs would have to be antacids. There is two groups of antacids: H2 Antagonists and Proton-Pump Inhibitors (PPIs).
In Australia, H2 Antagonists include Cimetidine (Tagamet); Ranitidine (Zantac); Famotidine (Pepcidine); and Nizatidine (Tazac).
PPIs are more popular no doubt due to their strength, and include Omeprazole (Losec); Esomeprazole (Nexium); Rabeprazole (Pariet); Pantoprazole (Somac); and Lansoprazole (Zoton).
Patients are filling medical clinics with acid reflux symptoms and out they walk with a prescription for some super dooper PPI.
Sadly, this is simply a band-aid to a problem which runs much deeper.
Sure it will give instant relief on the day and for a few weeks also, but in time, it will just be a curse to the patient who will rely on them ongoing.
Patients should be told the truth about their condition so hopefully, they can be empowered to make the appropriate changes in their diet and lifestyle. The medical profession owes them that.
So, here’s the truth from me.
When I first worked as a pharmacist, the only antacid on prescription was the H2 Antagonist, Tagamet (Cimetidine), and it had a LOT of drug interactions I must tell you. Soon after, Zantac (Ranitidine) came onto the market and pharmacists were much happier since it only had a handful of interactions at the time.
Both these drugs were hardly dispensed. Tagamet seemed to be given to chronic disease patients suffering from poor digestion due to multiple medications, whilst Zantac was mainly for pregnancy nausea or the occasional recovery from excessive food indulgence.
Indeed the most common antacid at the time was Mylanta mixture, and this was given mainly for overindulgence.
So basically, antacid prescriptions were only a small part of the overall drug industry at the time.
Boy, how that has changed today.
Losec (Omeprazole) was the first PPI to come to market in the early 90’s.
Since then, the antacid market has risen exponentially to an all-time high. It seems the majority of the public are on antacids, rather than the minority seen in the past. I dispense PPIs for approximately 1 in every 5 patients now.
So, why are people in need of so much acid reflux relief nowadays then?
It’s simply one word …. STRESS!
That dreaded word gets blamed for everything it seems right? Well, it certainly is the culprit for acid reflux no doubt.
Our society is working longer hours, with less downtime to relax and overstimulated into a constant ‘fight/flight’ mode. Our bodies feel ‘unsafe’, living daily in protective mode. We are ‘running’ from that virtual tiger about to eat us, even though in reality it may actually be sourced from a negative media report, financial burdens, pressure to meet deadlines or even marital strain for instance.
It is a known fact that STRESS LOWERS STOMACH ACID LEVELS.
But wait…if stress lowers stomach acid levels, why are stressed-out patients having acid reflux? Isn’t the problem from too much acid?
Great questions I say. To answer these, we first need to understand how the stomach controls acid levels.
The acid in the stomach is useful for breaking down foods, making them easier to digest, and also for helping prevent infection by providing an unfavourable environment for the growth of infective organisms. Normally, acid is secreted continuously in small amounts, with increased secretion in response to food intake.
Ideally, our bodies function best with a steady acid strength of say 8/10 maximum capacity. Stress can make our acid level in the stomach drop to a possible low 2/10 strength. Acid is secreted by parietal cells found in the stomach lining, involving a mechanism known as the proton pump. When food is ingested, the stomach realizes it has insufficient acid to digest the meal, so alarm bells ring and the proton pump quickly elevates the acid level.
Sadly, the acid level doesn’t just rise to a comfortable level of 8/10 strength. Instead, a mighty 15/10 strength level may be reached and the stomach can’t contain the pressure of this acid overload.
The stomach explodes acid out of it just like an explosive volcano, burning the oesophagus lining and giving the symptoms of acid reflux.
SO ACID REFLUX IS ACTUALLY A RESULT OF INCORRECT ACID LEVELS AT THE WRONG TIME IN RELATION TO MEALS.
PPIs work by permanently inactivating the proton pump responsible for acid secretion. They stop both the continuous secretion and secretion in response to food.
PPIs can decrease acid production by as much as 90%.
This is the culprit to a never-ending problem – low stomach acid as the cause of acid reflux has been ‘fixed’ with a drug that basically depletes all stomach acid secretion.
Makes no sense to me.
To say I’m frustrated by this type of prescribing and management is a true understatement.
Good stomach acid levels are vital for good health. I spend a great deal of time in clinic restoring stomach acid levels because I know how important this is for overall health.
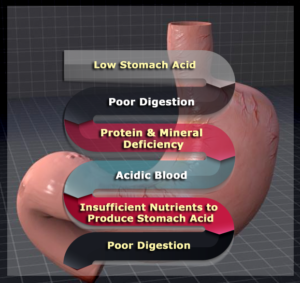
The Problem With Low Stomach Acid Levels
When the body is unable to produce enough stomach acid, it is unable to digest protein molecules and key minerals. These partially digested protein molecules get into the small intestine and create significant stress on the pancreas to produce adequate enzymes to metabolize the protein effectively.
If this occurs repeatedly over time, it will wear down the pancreatic enzyme storage and cause stress and irritation to the intestinal lining. Additionally, if the protein molecules are not efficiently metabolized we are unable to absorb enough amino acids which are necessary for numerous vital functions of the body. This can lead to amino acid deficiencies, poor healing and a breakdown of various important bodily functions.
The large protein molecules and incomplete digestion irritate the gut lining, leading to leaky gut syndrome. This process can trigger the development of autoimmune activity in the body. Poor digestion also creates an environment suited for the development of small intestinal bacterial overgrowth (SIBO), Candida overgrowth and parasitic infections.
When we digest our food poorly it leads to increased inflammatory activity which depletes key minerals and anti-oxidants throughout the body. This mineral depletion leads to an inability to form stomach acid and the vicious cycle of poor digestion and chronic inflammation continues.
Furthermore, low stomach acid prevents the activation of intrinsic factor which is a glycoprotein produced in the stomach that is necessary for vitamin B12 absorption.
Low stomach acid reduces the release of bile from the liver and gallbladder and digestive enzymes from the pancreas.
Interestingly, good stomach acid is an important trigger for the contraction of the oesophageal sphincter (just above the stomach) to protect the soft, delicate tissue of the oesophagus from the harsh acids in the stomach.
Good stomach acid also helps to activate the pyloric sphincter which allows food to move from the stomach to the small intestine.
So, good stomach acid levels prevent the volcano from erupting at all.
20 Signs that You Have Low Stomach Acid:
- Acid Reflux/Heartburn – as explained in this article is most commonly caused by low acid and not too much acid
- Digestive Discomfort (Indigestion, Bloating, Cramping, Gas, Belching) – due to gas production from bacterial fermentation in the stomach and is produced within an hour of eating
- Chronic Bad Breath
- Bad Body Odour – overall microbial overgrowth throughout the body
- Undigested Food in Stools
- Aversion to Meat
- Tired After Meals
- Feeling Full, But Still Hungry – food isn’t leaving the stomach, and nutrients aren’t absorbing effectively
- Chronic Anaemia/Vitamin B12 Deficiency – unable to absorb iron and Vitamin B12
- Weak Fingernails – a classic sign of nutrient deficiencies, especially protein, minerals and vitamin B12.
- Frequent Nausea
- Multiple Food Allergies/Sensitivities
- Dry Skin/Dandruff
- Candida Infections
- Acne
- Adrenal Fatigue – adrenals lack vital minerals for optimal function
- Hair Loss In Women
- Rectal Itching
- Diarrhoea/Constipation
- Osteoporosis & Other Autoimmune Disorders – poor calcium absorption and gut inflammation
How To Test For Low Stomach Acid?
- Mix 1/4 teaspoon of baking soda in half a glass of cold water, first thing in the morning before eating or drinking anything.
2. Drink the baking soda solution.
3. Time how long it takes for a burp or belch to come about. Wait for up to 5 minutes. If you have NOT burped or belched within 5 minutes, then it would be a sign of INSUFFICIENT stomach acid production.
10 Ways to Improve Stomach Acid Levels:
Reducing stress is a major factor in improving stomach acid levels. Lifestyle changes need to occur and more time for relaxation needs to incorporated into our daily routine.
Diet changes are especially important also and these tips will help improve your stomach acid levels:
- Use Liquid Nutrition Throughout the Day
You should ensure at least half of your meals are in a liquid form, such as a protein shake. Protein shakes are pre-metabolized and very easy to digest. They do not depend upon hydrochloric acid production, so they reduce stress on the GI system.
Drinking a mineral-rich tea (like nettle leaf) is valuable to ensure nutrients are being supplied to the body.
For more information, CLICK HERE read my article NETTLE LEAF TEA…NATURE’S MULTIVITAMIN
- Take Digestive Bitters
Bitters help to improve digestion and counter inflammation. Common examples include ginger, globe artichoke, dandelion root, golden seal, and olive leaf.
I commonly recommend drinking dandelion root tea and adding ginger to foods.
3. Super Hydrate Outside Of Meal Times
Good hydration will help activate bowel motility and push contents through the digestive system which will reduce microbial fermentation and toxicity in the body.
4. Drink Very Little With Meat Containing Meals
Anytime you are going to have meat or any heavy meal, you should cut off drinking water at least 30 minutes before the meal. This will reduce any potential dilution of the gastric juices and allow for better digestion.
5. Hold Off On Water After a Meal
To allow for optimal digestion, I recommend abstaining from water or liquids until at least 30 minutes after a meal. This allows for proper stomach acid activity, sterilization, protein metabolism, and more.
6. Use Lemon and Apple Cider Vinegar (ACV)
Using lemon juice or ACV on your meat and vegetables/salads helps to pre-metabolize the food. This allows for better digestion and nutrient absorption.
Lemon water and ACV contain organic acids that have an anti-microbial effect. So these help to reduce the bacterial load, especially the bacteria in the stomach such as H Pylori. Keeping H Pylori levels down is important for the body to be able to produce enough stomach acid.
Taking 1 teaspoon of ACV in 1/2 cup of water 30 minutes before a meal can increase vital stomach acid.
7. Use Fermented Vegetables
Fermented foods (such as sauerkraut, kimchi, gherkins) all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions. Aim to eat one of these with all of your heavier meals and especially any meal with protein.
- Increase Your Good Salt Intake
We need adequate amounts of chloride to produce hydrochloric acid. The best source of chloride is salt – Himalayan or Celtic sea salt to be exact.
People who are on salt-restricted diets end up compromised digestion.
Let’s not forget that these salts are also rich in over 80 minerals needed by the body.
For more information, CLICK HERE read my article TO SALT? OR NOT TO SALT?
Drink a good pinch of either of these salts dissolved in half a glass of water 30 minutes before each meal to increase stomach acid levels.
I usually combine salt and ACV for best results.
- Take Digestive Enzymes With Meals
Digestive enzymes will help you fully break down those nutrients you ingest, allowing you to replenish key nutrients to your body.
These can, of course, be combined with apple cider vinegar and salt for maximum benefit.
10. Eat Your Largest Meal When You Are Most Relaxed
In order to produce adequate stomach acid, your body needs to activate the parasympathetic nervous system. If you are busy and on the go, you will be in fight or flight sympathetic mode. If you struggle with low stomach acid, this is not going to allow you to produce anywhere near enough. Relaxing before the meal is key to improve stomach acid production. Also, aim to chew more to aid digestion further too.

By following these strategies, you reduce stress on our digestive system and absorb nutrients more effectively. This will help your body to have the resources it needs to produce adequate stomach acid in the future.
Make sure you work with a natural practitioner who can guide you through the process and offer suggestions for a healthy eating plan along the way. The practitioner may also suggest adding some Betaine HCL with pepsin supplementation to encourage stomach acid levels to lift more quickly.
More importantly, the practitioner will need to rule out any underlying conditions often masked by similar symptoms.
When you improve stomach acid levels, it makes a huge difference in your overall health and quality of life.
**If you’ve got this far – thank you for reading and I look forward to bringing you more information in the future.